The Findings
Policy Recomandations for SUD Recovery Project Findings
Project Findings
Research indicates the importance of peer recovery specialists to SUD recovery. Increasing the number of specialists will depend on higher salaries, in part through increased Medicaid reimbursement rates, and on legislation to repeal barrier crime bans for Virginia Department of Behavioral Health and Developmental Services employees who do not serve children or people with intellectual disabilities.
Virginia needs to establish more pathways to treatment for those who encounter the criminal justice system, including more non-arrest pathways. The Project RECOVER pilot program in Richmond, Virginia, which employs peer recovery specialists to co-respond alongside law enforcement officers, will hopefully become available statewide.
There is an increased need to expand harm reduction measures including more needle exchange programs, more naloxone distribution, and a mobile harm reduction unit for localities that qualify, including the City of Radford, Pulaski County, and Giles County in the New River Valley.
Southwest Virginia needs affordable broadband internet for access to telehealth services.
Addressing all of these priorities depends upon decreasing stigma surrounding mental illness and Substance Use Disorder. Greater awareness that SUD is a disease not a crime will encourage more people to seek recovery and will enable advocates to garner more support from legislators and local communities.
SUD Recovery Facilties
In Virginia, state-run hospitals are experiencing an extreme staffing crisis and many facilities are in need of repair or restoration. It is clear that expansion of recovery services will not be possible without first addressing lack of funding for mental and behavioral health services more broadly. If that initial need can be met, then it becomes possible to focus on providing more facilities for residential and outpatient treatment and recovery services.
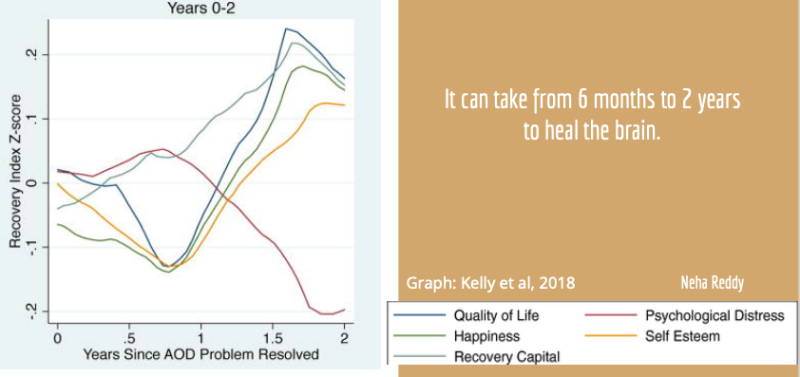
For those diagnosed with substance use disorder, it can take 6 months to 2 years to heal the brain. A mix of short-term and long-term support is required, especially during the first 12 months-- as shown in the graph below which charts plummeting quality of life, happiness, and self esteem in the first year following resolution of drug disorders.
Listed below are the wide variety of recovery facilities needed for SUD recovery. According to our key informants in the New River Valley, people in recovery need medically-observed treatment before they are eligible for long-term recovery housing such as Oxford House, yet there are only 10 in-patient beds in our CSB. The Housing First model could provide another route as it emphasizes immediate access to housing without preconditions such as sobriety. Also needed, according to key informants, are long-term supportive housing, permanent supportive housing, and housing for families, among others. One reason that the need for state-run facilities is so dire is due to the high cost of care, which most individuals are unable to afford. Inpatient treatment facilities can cost $14,000 to $27,000 for a 30-day program. Outpatient treatment can range from free to five hundred dollars ($500) per session.
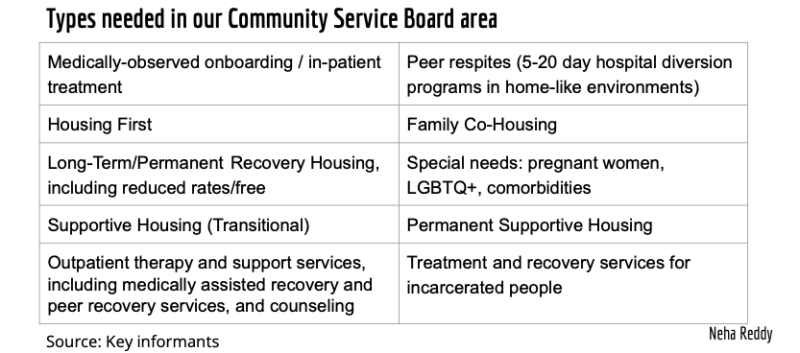
Our key informants stated a need for expansion of recovery housing options for a wider range of individuals, including options for families, pregnant mothers, members of the LGBTQ+ community, and individuals with co-morbidities. Many current housing options are only available to people further along on their recovery journey, are not welcoming of Medically Assisted Recovery, and/or have prohibitive out-of-pocket costs.
An article in the Journal of Nursing Scholarship features one model in Ohio that improved recovery rates for patients following overdoses. The Maryhaven Center includes three levels of care: triage and admission, withdrawal management, and residential treatment equipped with a variety of counseling options, some led by peer recovery specialists, and medically assisted recovery. This center is quite successful with 63.5% of patients completing withdrawal management, and 73.4% completing the residential program. Our informants recommend facilities supporting even longer-term programs, including recovery housing and peer respites for occasional short-term stays.
Recovery is a multi-year process, and patients need support through each stage.


